Vaccination Programme for Bucks
Buckinghamshire Council has published the following detailed account of the Covid vaccination programme for the county
Covid-19 Vaccination Programme
Status as at Tuesday 12th January 2021
Summary of latest information
Number of residents vaccinated to 12 January 2021: approximately 12,000
Two additional GP led vaccination sites will launch this week in Aylesbury and Central Wycombe bringing the total number of local sites to 7
Hospital Hub for health & social care staff managed by Buckinghamshire Healthcare NHS Trust was launched last week with a 7-day operation. 1,950 vaccines have been delivered.
Two Pharmacy led sites across Buckinghamshire confirmed and to go live from 18th January with additional ones being planned.
National mass vaccination site programme has started.
The Plan
The Government has announced that the top four priority groups in the Joint Committee for Vaccination and Immunisation (JCVI) list will be completed by mid-February.
These are:
1. Residents in a care home for older adults and their carers
2. All those 80 years of age and over and frontline health and social care workers
3. All those 75 years of age and over
4. All those 70 years of age and over and clinically extremely vulnerable individuals
This is around 120,000 people in Buckinghamshire, and we expect to deliver vaccinations for all 4 priority groups by the middle of-February.
There are a number of different routes through to vaccination:
- Local Vaccination Sites (run by Buckinghamshire GPs). GPs are also delivering the vaccine directly to care homes for their residents and staff.
- Pharmacy Sites
- National mass vaccination sites
- Hospital sites for health and social care staff
In Buckinghamshire, all GP Led sites are expected to be operating by 25 January and all residents over the age of 80 will be offered a vaccination appointment locally through their GP Practice by the end of January.
How the rollout is going in Buckinghamshire
Vaccination sites already underway
All GPs are involved in the rollout of the vaccination programme, through eight GP led sites across the county.
Please note that vaccinations are not delivered at GP surgeries but at the vaccination site they are linked to.
Chalfont Local Vaccination Site
This site will administer the vaccine to eligible patients registered at:
Iver Medical Centre
Threeways Surgery
Burnham Health Centre
Southmead Surgery
Denham Medical Centre
The Hall Practice
The Misbourne Practice
The Allan Practice
Little Chalfont Surgery
Chesham Local Vaccination Site
This site will administer the vaccine to eligible patients registered at:
The New Surgery
Water Meadow Surgery
Gladstone Road Surgery
Rectory Meadow Surgery
Amersham Health Centre
John Hampden Surgery
Hughenden Valley Surgery
Prospect House Surgery
High Wycombe Local Vaccination Site
This site will administer the vaccine to eligible patients registered at:
Millbarn Medical Centre
Highfield Surgery
Marlow Medical Centre
Cherrymead Surgery
The Simpson Centre
Bourne End & Wooburn Green Medical Centre
Tower House Surgery
Desborough Surgery
Kingswood Surgery
Priory Surgery
Princes Risborough Local Vaccination Site
This site will administer the vaccine to eligible patients registered at:
Cross Keys Surgery
Unity Health
Winslow Local Vaccination Site:
This site will administer the vaccine to patients eligible registered at:
Ashcroft Surgery
Waddesden Surgery
3W Health
The GP will either call residents or send them a letter inviting them to your appointment.
We are asking that no one calls their GP or goes to the vaccination site without an invitation
New vaccination sites
Two further sites are going live on Friday 15th January as follows:
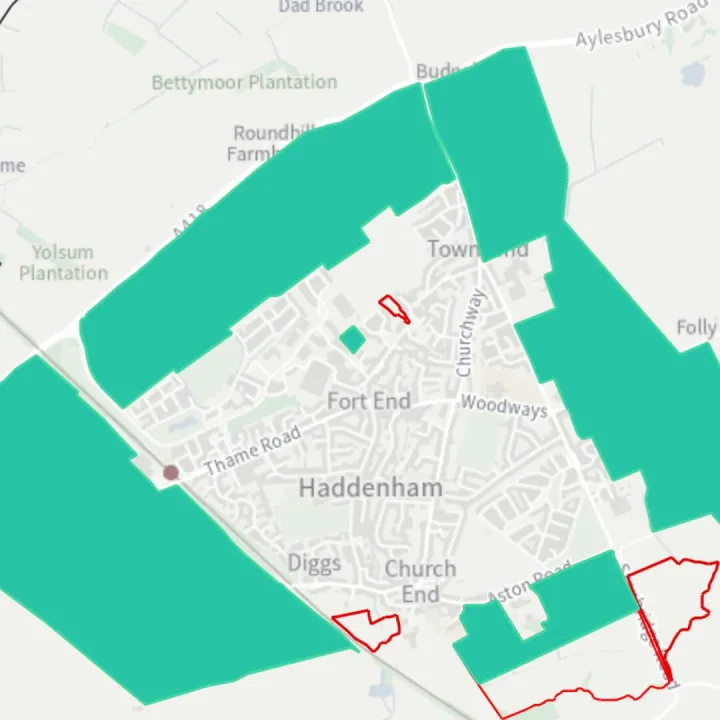
Aylesbury Local Vaccination Site
This site will administer the vaccine to eligible patients registered at:
Berryfields Medical Centre
Edlesborough Surgery
Haddenham Medical Centre
Mandeville Surgery
Meadowcroft Surgery
Oakfield Surgery
Poplar Grove Practice
Westongrove PCN
Whitehill Surgery
High Wycombe Town Centre Local Vaccination Site:
This site will administer the vaccine to eligible patients registered at:
Carrington House Surgery
Chiltern House Medical Centre
Riverside Surgery
Riverside Surgery
Stokenchurch Medical Centre
Wye Valley Surgery
Buckingham (for The Swan Practice) will start vaccinating shortly.
A further site is being planned for the south of the county.
All Buckinghamshire GP Led sites will be operating by 25th January and all residents over the age of 80 will be offered a vaccination appointment at one of the local vaccination sites through their GP Practice by the end of January.
National Mass Vaccination Sites booked via the National Booking system
In addition to the local vaccination sites, the NHS is setting up some national mass vaccination sites.
Currently, the sites currently closest to Buckinghamshire are:
Epsom racecourse in Surrey (South East)
Excel Centre in London (London)
Robertson House in Stevenage (East of England)
Letters from the NHS begun arriving this weekend to people aged 80 or over who live 30 to 45 minutes' drive from one of the seven new national sites, including residents who live in Buckinghamshire. The letter explains how they can book a slot – over the phone or online through the national booking service.
Buckinghamshire residents who have received the letter can choose to book through the national booking system if they do not want to use the local system.
However, all patients over the age of 80 will be offered a vaccination appointment locally through their GP Practice by the end of January. If residents do not want to attend one of these Mass Vaccination sites, it will not affect their ability to get an appointment at a local site through their GP.
We are aiming to have two Mass Vaccination sites in Buckinghamshire (Aylesbury and Wycombe). Residents will be able to book your vaccination through the National Booking system. More information will be made available in the coming week.
Pharmacy led sites
Residents should soon be able to book to have their vaccination through three pharmacy vaccination sites using the National Booking system
Marlow – expected to go live week beginning 18th January.
Wycombe – expected to go live week beginning 18th January.
Buckingham – expected to go live week beginning 25th January.
Further sites are being commissioned by the NHS and more information will be made available in the coming week.
Patients will have a choice of attending either a GP led site, or a pharmacy led site if that is more convenient.
Additional Information
Attached are the latest FAQs from the NHS on the vaccination programme.
There is also now a section on the Council's website about the Vaccination programme which will be updated regularly. Vaccine programme
FAQs
Most popular
What vaccine for COVID-19 is currently available?
Both the Pfizer/BioNTech and Oxford/AstraZeneca COVID-19 vaccines are now available. Both vaccines have been shown to be safe and offer high levels of protection and have been given regulatory approval by the MHRA.
The Government has in principle secured access to seven different vaccine candidates, across four different vaccine types, totalling over 357 million doses. This includes:
- 40 million doses of the BioNTech/Pfizer vaccine
- 100m doses of the Oxford/AstraZeneca vaccine.
- 7 million doses of the Moderna vaccine, which is also being assessed by the MHRA.
Is the NHS confident the vaccines are safe?
Yes. The NHS will not offer any Covid-19 vaccinations to the public until independent experts have signed off that it is safe to do so.
The MHRA, the official UK regulator, have said that both of these vaccines have good safety profiles and offer a high level of protection, and we have full confidence in their expert judgement and processes.
As with any medicine, vaccines are highly regulated products.
There are checks at every stage in the development and manufacturing process, and continued monitoring once it has been authorised and is being used in the wider population.
Will the vaccines work with the new strain?
There is no evidence currently that the new strain will be resistant to the vaccines we have, so we are continuing to vaccinate people as normal. Scientists are looking now in detail at the characteristics of the virus in relation to the vaccines. Viruses, such as the winter flu virus, often branch into different strains but these small variations rarely render vaccines ineffective.
Why are you postponing second doses?
The UK Chief Medical Officers have agreed a longer timeframe between first and second doses so that more people can get their first dose quickly, and because the evidence shows that one dose still offers a high level of protection.
This decision will allow us to get the maximum benefit for the most people in the shortest possible time and will help save lives.
We recognise for some people a longer wait might be worrying, and clinicians have the discretion to vaccinate people sooner if they think this is needed. Getting both doses remains important so we would urge people to return for it at the right time.
Why are healthcare workers amongst the first groups to receive the vaccine?
The JCVI have put patient-facing health and social care staff into a priority group because of their heightened risk of exposure to the virus. Healthcare workers are not the top priority though, and with limited vaccine available up to now, employers have been asked to offer the vaccine to the most at risk healthcare workers first. With many more doses now expected over the coming weeks, employers will be widening this out and protecting staff as soon as possible.
The NHS is experienced in vaccinating hundreds of thousands of staff quickly and safely – we do it every year for the flu vaccine – and all local NHS employers will be responsible for ensuring that 100% of eligible staff have the opportunity to take it up over the coming weeks and months.
Why aren't all healthcare workers getting vaccinated right now?
The Government have confirmed that the vast majority of vaccinations administered by the NHS in this initial phase will be prioritised for those 80 years of age and over and care home residents and workers.
Up to now some staff have been vaccinated to avoid doses going to waste, with employers asked to identify those who can benefit most to go first using the risk assessment framework to identify those at greatest risk. Over the following days and weeks as we get more supplies this will continue to be rolled out.
How will healthcare workers get the vaccine?
The NHS will offer vaccinations using different models. For healthcare workers, dozens of NHS trusts will act as hospital hubs where NHS staff can get vaccinated on site.
Will you use the Oxford/AstraZeneca vaccine more because it's cheaper and easier to store?
The vaccines that the NHS uses and in what circumstances will be decided by the MHRA. Both vaccines are classed as being very effective. The Oxford/AstraZeneca is easier to store and transport, meaning we can deliver them in more places, and we expect to have more doses available as they are manufactured in the UK, so we would expect that most people are likely to receive this vaccine over the coming weeks and months.
Should people who have already had Covid get vaccinated?
Yes, if they are in a priority group identified by JCVI. The MHRA have looked at this and decided that getting vaccinated is just as important for those who have already had Covid-19 as it is for those who haven't.
Do I need to leave a space between having the flu vaccine and having the Covid vaccine?
It is not essential to leave time between the flu and Covid vaccine but it is recommended that there should be a gap of a week.
We would always encourage anyone who is eligible but not yet taken up their flu jab to do so as soon as possible.
Can people pick what vaccine they want?
Any vaccines that the NHS will provide will have been approved because they pass the MHRA's tests on safety and efficacy, so people should be assured that whatever vaccine they get, it is worth their while.
If a household has a priority group member, such as an NHS frontline worker or vulnerable person, will everyone living in that household be vaccinated together?
These decisions are for the JCVI. Their current prioritisation plan does not include household members of NHS staff or clinically vulnerable people automatically – although in some cases family members may be eligible in their own right.
Can I get one privately?
No. Vaccinations will only be available through the NHS for the moment. Anyone who claims to be able to provide you with a vaccine for a fee is likely to be committing a crime and should be reported to the Police online or by calling 112.
Is one vaccine better than the other?
The important point for any vaccine is whether the MHRA approves it for use – if it does then that means it's a worthwhile vaccine to have and people should have it if they are eligible. Data from clinical trials does suggest the Pfizer vaccine offers marginally more protection, but both are classed as highly effective.
Who gets the vaccine first?
The Joint Committee for Vaccination and Immunisation (JCVI) published its final advice on 2nd December which can be found here: https://www.gov.uk/government/publications/prioritygroups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-2-december2020/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-2-december-2020
The Government has confirmed that the vast majority of vaccinations administered in this initial phase will be prioritised for those 80 years of age and over, and care home workers.
Vaccinating services should therefore ensure any unfilled appointments are used to vaccinate healthcare workers, from across their local healthcare system, who have been identified at highest risk of serious illness from COVID-19. Healthcare providers have been undertaking staff risk assessments throughout the pandemic to identify such individuals.
Has the MHRA approved care home jabs?
Yes, this has been approved and the NHS has been working through the delivery mechanism to ensure we can safely break up batches, transport it and deliver it in care homes. The roll out to care homes has now started.
Can any member of the public be vaccinated? Can they just walk in to a service?
People will be offered vaccinations in line with recommendations from the independent JCVI. The NHS will contact people when it is their turn. People will need an appointment to get their vaccine; most people will be invited by letter from their GP practice or the national programme.
How many vaccines are you expecting to do by the end of January?
The most important thing is that the NHS aims to vaccinate as many people as safely and quickly as possible – staff are delivering something new so there is no benefit to putting arbitrary targets on it now. However, we have made an excellent start to the programme, delivering over three quarters of a million in just under three weeks, and having an additional vaccine will allow us to go further and faster over the coming weeks.
Vaccine safety
Is the NHS confident the vaccine is safe?
Yes. The NHS will not offer any Covid-19 vaccinations to the public until independent experts have signed off that it is safe to do so.
The MHRA, the official UK regulator, have said these vaccines are safe and highly effective, and we have full confidence in their expert judgement and processes.
As with any medicine, vaccines are highly regulated products.
There are checks at every stage in the development and manufacturing process, and continued monitoring once it has been authorised and is being used in the wider population.
The MHRA recommend that those with severe allergies to the ingredients of the vaccines should not receive them.
Are there any side effects?
These are important details which the MHRA always consider when assessing candidate vaccines for use.
For these vaccines, like lots of others, they have identified that some people might feel slightly unwell, but they report that no significant side effects have been observed in the tens of thousands of people involved in trials.
All patients will be provided with information on the vaccine they have received, how to look out for any side effects, and what to do if they do occur, including reporting them to the MHRA.
More information on possible side effects can be found at https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/coronavirus-vaccine/
When will you publish vaccine ingredients?
A detailed review of the vaccines and their ingredients have been provided by the MHRA and can be found at the following links.
For the Pfizer/BioNTech vaccine information is available here: https://www.gov.uk/government/publications/regulatory-approval-of-pfizer-biontech-vaccine-for-covid-19
For the Oxford/AstraZeneca vaccine information is available here: https://www.gov.uk/government/publications/regulatory-approval-of-covid-19-vaccine-astrazeneca
The British Islamic Medical Association have produced a helpful guide for the Muslim community which can be found at https://britishima.org/pfizer-biontech-covid19-vaccine/
What about the allergic reactions that have been reported?
These vaccines are safe and effective for the vast majority of people – they have been tested on tens of thousands of people and assessed by experts.
Any person with a history of immediate-onset anaphylaxis to the ingredients contained in the vaccines should not receive them. A second dose of the Pfizer/BioNTech vaccine should not be given to those who have experienced anaphylaxis to the first dose of Pfizer/BioNTech vaccination.
Everybody will also be screened for potential allergic reactions before getting vaccinated. All vaccinators will have the training they need to deal with any rare cases of adverse reactions, and all venues will be equipped to care for people who need it – just like with any other vaccine.
Has the guidance on allergies changed?
The original MHRA advice was that anybody with a known allergy to specific ingredients in the vaccine should not be vaccinated. This was temporarily widened but the guidance has now reverted to this.
Checking for allergies is a routine part of the process before giving any vaccine or new medicine. Having these conversations – as well as being able to deal with allergic reactions in the rare case they do happen, is a central part of training for vaccinators. But these are new vaccines and so the NHS and the MHRA are being extra vigilant and responding quickly to ensure everyone across the NHS is totally clear on these requirements.
How effective are the vaccines? How long do they take to work?
The MHRA have said these vaccines are highly effective, but to get full protection people need to come back for the second dose – this is really important.
To ensure as many people are vaccinated as quickly as possible, the Department for Health and Social Care now advise that the second dose of both the Oxford AstraZeneca and the Pfizer/BioNtech vaccine should be scheduled up to 12 weeks apart.
Full protection kicks in around a week or two after that second dose, which is why it's also important that when you do get invited, you act on that and get yourself booked in as soon as possible. Even those who have received a vaccine still need to follow social distancing and other guidance.
What happens if a person has the first jab but not the second?
Both vaccines have been authorised on the basis of two doses because the evidence from the clinical trials shows that this gives the maximum level of protection.
To ensure as many people are vaccinated as quickly as possible, the Department for Health and Social Care now advise that the second dose of both the Oxford/AstraZeneca and the Pfizer/BioNtech vaccine should be scheduled up to 12 weeks apart.
The evidence doesn't show any risk to not having the second dose other than not being as protected as you otherwise would be. We would urge everyone to show up for both of their appointments for their own protection as well as to ensure we don't waste vaccines or the time of NHS staff.
Does the vaccine include any parts from foetal or animal origin?
There is no material of foetal or animal origin in either vaccine. All ingredients are published in healthcare information on the MHRA's website.
For the Pfizer/BioNTech vaccine information is available here: https://www.gov.uk/government/publications/regulatory-approval-of-pfizer-biontech-vaccine-for-covid-19
For the Oxford/AstraZeneca vaccine information is available here: https://www.gov.uk/government/publications/regulatory-approval-of-covid-19-vaccine-astrazeneca
How does the vaccine work?
The vaccine works by making a protein from the virus that is important for creating protection.
The protein works in the same way they do for other vaccines by stimulating the immune system to make antibodies and cells to fight the infection.
How long will my vaccine be effective for?
We expect these vaccines to work for at least a year – if not longer. This will be constantly monitored.
Are there any groups that shouldn't have the vaccine?
People with history of a severe allergy to the ingredients of the vaccines should not be vaccinated.
The MHRA have updated their guidance to say that pregnant women and those who are breastfeeding can have the vaccine but should discuss it with a clinician to ensure that the benefits outweigh any potential risks.
Does the vaccine work on those taking immune suppressants?
Although the vaccine was not tested on those with very serious immunological conditions, the vaccine has been proven to be very effective and it is unlikely that the vaccine will have no effect at all on these individuals.
There may be a very small number of people with very complex or severe immunological problems who can't make any response at all – but the vaccine should not do any harm to these individuals. Individuals meeting these criteria may want to discuss the vaccine further with their specialist doctor.
Delivering the vaccine
How is the NHS delivering vaccines?
The NHS will offer vaccinations using three different models. In the first instance, dozens of NHS trusts are acting as hospital hubs where the vaccine can be stored safely and where many in the top priority groups - including the over 80s, care home workers and at-risk NHS staff – have been able to get vaccinated on site.
To make it as easy as possible for those who are eligible to access a vaccination safely, hundreds of Local Vaccination Services have been set up, with more due to start in the coming weeks. These community and primary care-led services will vary based on local and logistical considerations but include GP practices, local authority sourced buildings or other local facilities, as well as roving teams who have started delivering it in some care homes.
When the supply of doses allows, the NHS will also establish vaccination centres, where large numbers of people will be able to go and get vaccinated. These could be in local venues such as sports stadiums, racecourses, and concert venues that offer the physical space to deal with large numbers of people while maintaining social distancing.
Do vulnerable people travel to get the vaccine or does it come to them?
We are planning a mixed approach to ensuring that people who are eligible can get the vaccine safely. For care home residents and those who can't leave home, this will involve roving community teams coming to them.
How will patients be invited for a vaccination? How/when will they go for the second? Will this be at the same place/what happens if there is a delay in between?
When it is the right time people will be contacted to make their appointments. For most people they will receive a letter either from their GP or the national booking system; this will include all the information they need, including their NHS number. Some services are currently also phoning and texting patients to invite them in.
We know lots of people will be eager to get protected but we would ask people not to contact the NHS to get an appointment until they are contacted. The NHS is working hard to make sure those at greatest risk are offered the vaccine first.
When you book your first dose you will also be asked to book your second too. For most people this will be within three months of your first dose. The UK Chief Medical Officers have agreed this longer timeframe so that more people can get their first dose quickly, and because the evidence shows that one dose offers a high level of protection. Getting both doses remains important so we would urge people to return for it at the right time.